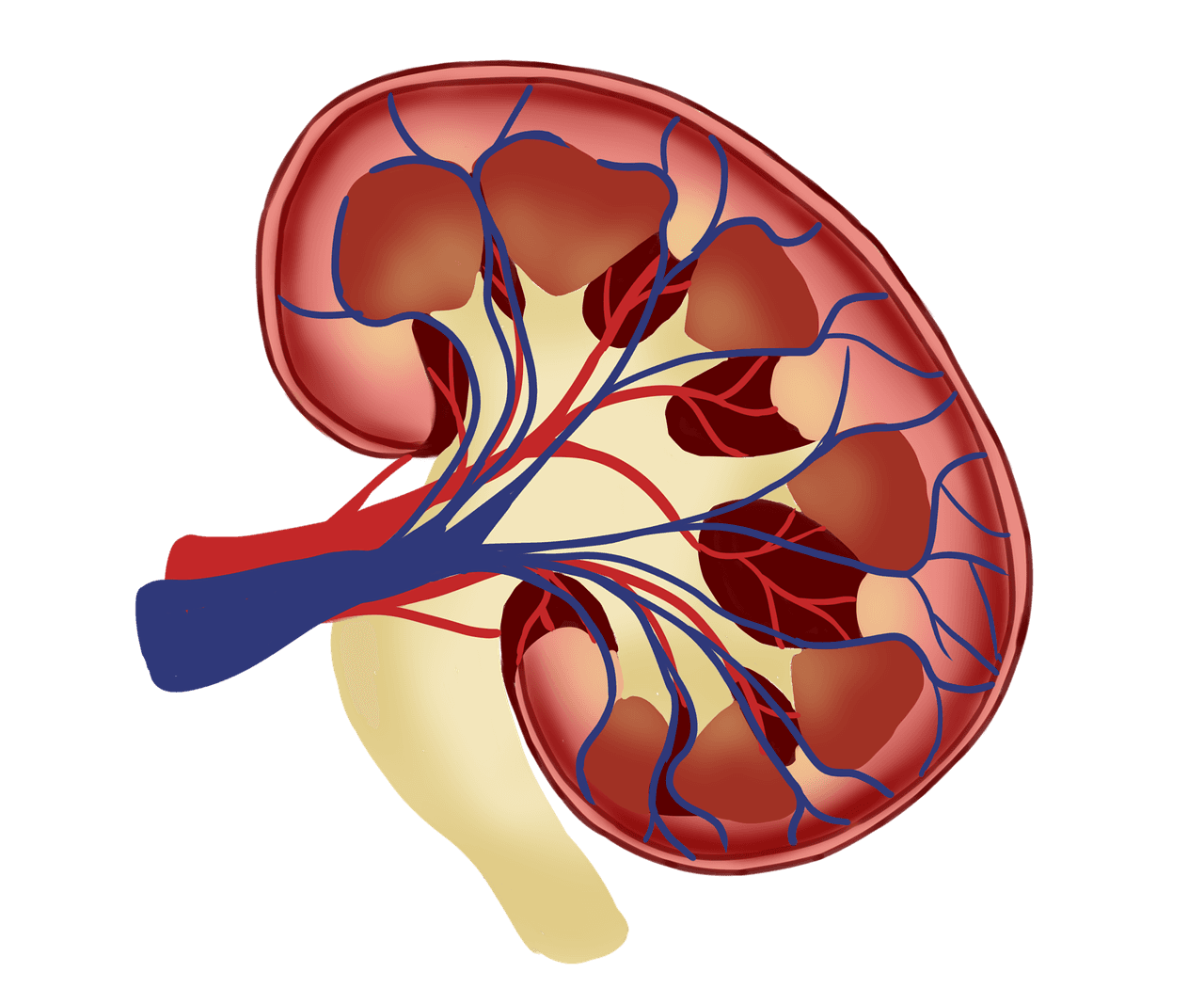
Kidney Disease
Renal nutrition therapy for chronic kidney disease management and dialysis support.
Chronic kidney disease (CKD) requires specialized medical nutrition therapy to slow disease progression, manage uremic symptoms, and prevent complications. Nutritional management must be carefully individualized based on CKD stage, presence of diabetes or hypertension, and treatment modality (conservative management, hemodialysis, peritoneal dialysis, or transplantation). Therapeutic diets focus on controlling protein, sodium, potassium, phosphorus, and fluid intake while maintaining nutritional adequacy and preventing malnutrition.
Clinical Focus
Protein restriction (0.6-0.8g/kg/day) in early-stage CKD to slow progression, with adjustments for dialysis patients (1.2-1.4g/kg/day).
Phosphorus restriction (<800-1000mg/day) through limitation of high-phosphorus foods and phosphate binders when indicated.
Potassium and sodium management based on laboratory values, fluid status, and blood pressure, with restrictions typically <2,000-2,500mg/day for potassium.
Monitoring and managing protein-energy wasting through regular assessment and nutritional support interventions.
Key Points
Individualized macronutrient and micronutrient goals based on CKD stage, GFR, and laboratory parameters (creatinine, BUN, potassium, phosphorus).
Plant-dominant dietary patterns with controlled protein intake shown to slow CKD progression and reduce cardiovascular risk.
Careful fluid management (typically 1-2L/day) for patients with fluid retention or on dialysis.
Coordination with nephrology team for comprehensive management including medication-nutrient interactions and dialysis adequacy.